Is nutritional psychiatry another tool to help improve mental health or is it just another fad pushed by the media?
The field of study known as nutritional psychiatry is a relatively new concept in modern healthcare. With many new research projects taking place on the quality of food intake and its association with mental health. There is increased interested in the effectiveness of a quality diet on mental health.
The idea that “food is medicine” is prevalent in the mainstream media, and seemingly being pushed in an act of rebellion against the pharmaceutical companies. This idea is rather convincing, with celebrities pushing catch phrases like “clean”, “homeopathic”, “cleansing”, and “detox”, and documentaries claiming that eating patterns can cure everything from the common cold to heart disease. It can be hard to determine where the truth is. Many of these claims are pseudoscience or outright false. Nutritional psychiatry, on the other hand, is relatively new and few claims have been made in the media. So what does the research say?
The research
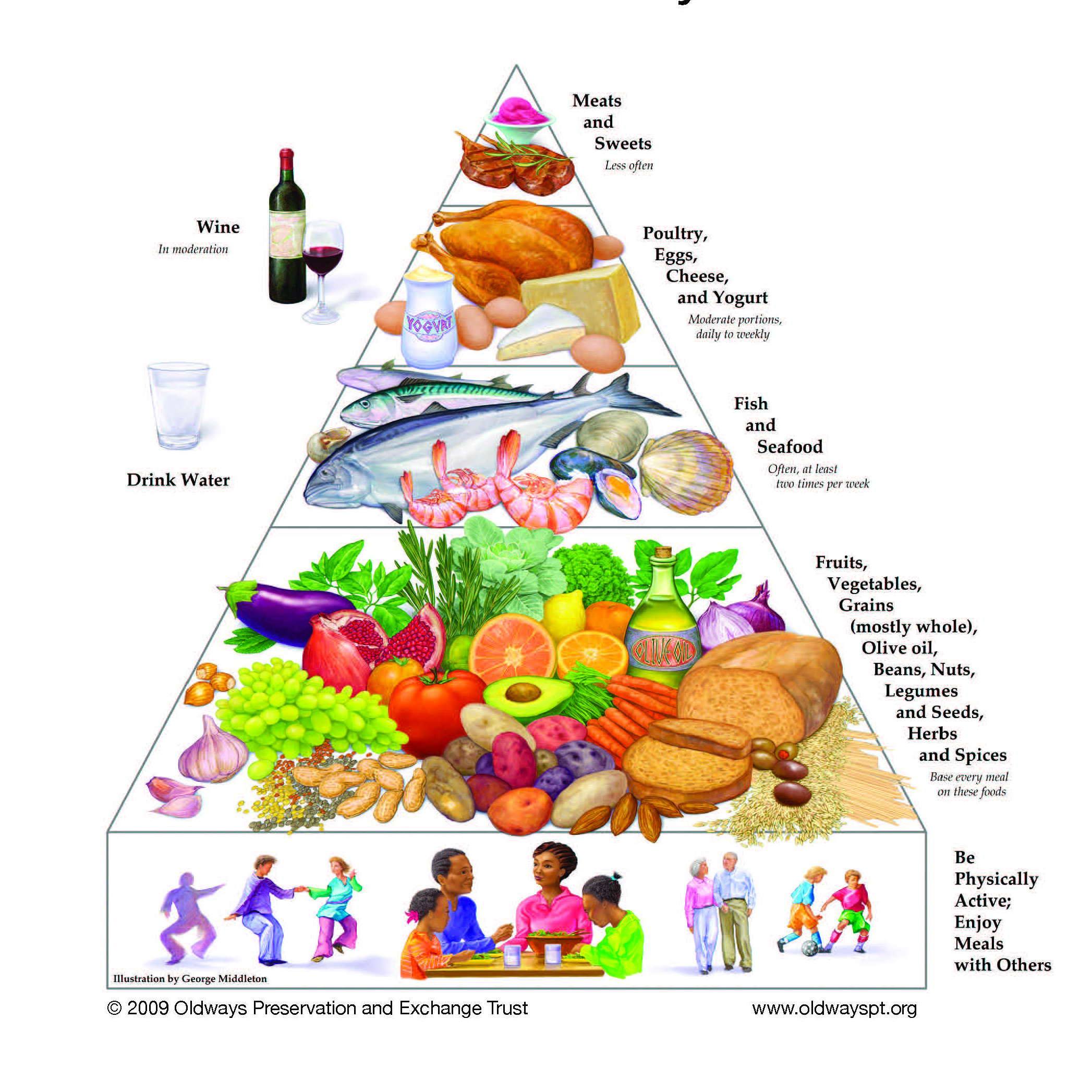
The first study done to explore dietary intake and clinical depression is known as the SMILES (Supporting the Modification of lifestyle in Lowered Emotional States) trial. This trial was meant to specifically answer the question “If I improve my diet, will my mental health improve”. A modified Mediterranean diet led by a clinical dietitian was used in this randomized control trial and the results suggested that eating a Mediterranean styled diet can decrease symptoms of depression (Jacka, et al., 2017).
Another study has since followed up on these findings, with similar results. Parletta et al. (2019) used a Mediterranean styled diet supplemented with fish oil, and found significant reductions in depression for participants in the diet group. Another noteworthy study, the PREDI-MED trial, is currently underway. This study will use a Mediterranean styled diet to determine the long term effects of the Mediterranean diet on the prevention of recurrent depression (Sánchez-Villegas et al., 2019).
Anxiety, which often goes hand in hand with depression, is another topic under discussion. There is currently very little research using human trials that account for diet when assessing mood. However, there have been successful trials in rodents, which have shown that differences in gut microbiota can be linked to anxiety (Taylor et al., 2020). As well, a more recent study out of the Netherlands revealed that higher intakes of vegetables and non-refined grains corelated with a lower risk of depression and anxiety severity. A curious finding from this study was that higher intakes of poultry and high-fat dairy was associated with increased symptoms of depression and anxiety, while a higher consumption of red meats was associated with decreased symptoms (Gibson-Smith et al., 2020).
The results
 While research is ongoing in this field, the general consensus is that mental health benefits from a whole food diet (such as the Mediterranean diet) and is impacted less by single nutrient additions to the diet (such as supplements). This is likely because nutrients in foods exist in combination with other nutrients; this complexity is suspected to be the factor that leads to better mental health outcomes. It is known that supplementation combined with a healthy diet (the addition of fish oil), or a healthy diet combined with medications, leads to better outcomes (Taylor et al., 2020). It is also worth noting that nutrient deficiencies can have an effect on mental health, including cognitive impairments and depressive symptoms resulting from a B12 deficiencies (Esnafoglu & Ozturan, 2020), or the increased autistic traits that are often expressed in women with anorexia (Tchanturia et al., 2019).
While research is ongoing in this field, the general consensus is that mental health benefits from a whole food diet (such as the Mediterranean diet) and is impacted less by single nutrient additions to the diet (such as supplements). This is likely because nutrients in foods exist in combination with other nutrients; this complexity is suspected to be the factor that leads to better mental health outcomes. It is known that supplementation combined with a healthy diet (the addition of fish oil), or a healthy diet combined with medications, leads to better outcomes (Taylor et al., 2020). It is also worth noting that nutrient deficiencies can have an effect on mental health, including cognitive impairments and depressive symptoms resulting from a B12 deficiencies (Esnafoglu & Ozturan, 2020), or the increased autistic traits that are often expressed in women with anorexia (Tchanturia et al., 2019).
It’s important to recognize that there is no magic pill, or one-size-fits-all solution to the growing prevalence of mental health disorders. As future studies evolve and conduct human trials on the gut microbiota in relation to diet, more information will be gathered to better predict the outcome of food on mood disorders. In the meantime, there is no harm in eating a healthy diet. Diets low in sugar and high in fatty acids are recommended, and eating complex carbohydrates and maintaining a diet high in fruits, vegetables, and whole grains can be a healthy way to manage symptoms. As well, there is evidence that the antioxidant Vitamins A, C, and E protect against cognitive function and mental disorders, including anxiety.
Was this article helpful? Have more questions? Tell me about it in the comments!
References
Jacka, F.N., O’Neil, A., Opie, R. et al. (2017). A randomized controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med, 15, 23. https://doi.org/10.1186/s12916-017-0791-y
Parletta, N., Zarnowiecki, D., Cho, C., et al. (2019). A Mediterranean-style dietary intervention supplemented with fish oil improves diet quality and mental health in people with depression: A randomized controlled trial (HELFIMED). Nutritional Neuroscience, 22(7), 474-487. DOI: 10.1080/1028415X.2017.1411320
Sánchez-Villegas, A., Cabrera-Suárez, B., Molero, P. et al. (2019). Preventing the recurrence of depression with a Mediterranean diet supplemented with extra-virgin olive oil. The PREDI-DEP trial: study protocol. BMC Psychiatry, 19, 63. https://doi.org/10.1186/s12888-019-2036-4
Taylor, A. M., & Holscher, H. D. (2020). A review of dietary and microbial connections to depression, anxiety, and stress. Nutritional Neuroscience. 23(3), 237–250. doi: 10.1080/1028415X.2018.1493808.
Gibson-Smith, D., Bot, M., Brouwer, I.A. et al. (2020). Association of food groups with depression and anxiety disorders. Eur J Nutr. 59, 767–778. https://doi.org/10.1007/s00394-019-01943-4
Tchanturia, K., Adamson, J., Leppanen, J., & Westwood, H. (2019). Characteristics of autism spectrum disorder in anorexia nervosa: A naturalistic study in an inpatient treatment programme. Autism, 23(1), 123–130. https://doi.org/10.1177/1362361317722431
Esnafoglu, E., & Ozturan, D. (2020). The relationship of severity of depression with homocysteine, folate, vitamin B12, and vitamin D levels in children and adolescents. Child and Adolescent Mental Health. 25(4), 249-255. https://doi.org/10.1111/camh.12387
- 1,2,3’s of Building Strong Bones in Adolescent Girls - January 7, 2021
- Chewy Trail Mix Cookies - December 21, 2020
- Nutritional Psychiatry: One More Tool in the Toolbox? - December 18, 2020